Herbal Blends Submenu
What Are Biofilms?
 |
Electron microscope view of bacteria (green) hiding within a tough biofilm matrix (brown). |
One reason why infections like C. difficile can be so challenging to treat is because of biofilms. Biofilms are like an armored plating that bacteria make to protect themselves inside your body or on surfaces in the environment. This tough protective "skin" helps shield colonies of bacteria from antibiotics and other treatments, giving them a place to hide, breed and grow.
Biofilms are so common that you probably see them every day and don't even realize it. The slimy layer inside your pet’s water dish that's so hard to clean is a biofilm. The hard dental plaque on your teeth is another type of biofilm. Biofilms are a defensive hiding place that help bacteria to survive and shield themselves from antibiotic drugs.
Biofilms also serve as a resevoir for bacteria in your body to infect you. C. diff. bacteria can hide inside biofilms long after your antibiotic treatment has ended, waiting for ideal conditions to cause another infection. Biofilms can survive in many parts of your body and go undetected for long periods of time.
Biofilms and Recurring Infections
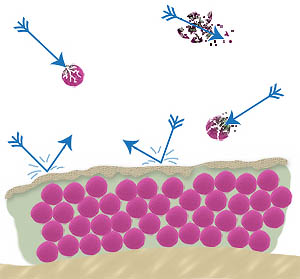 |
Depiction of a biofilm cross-section. Bacteria (pink) inside a biofilm are protected from antibiotic drugs (arrows). But free-floating bacteria outside of the biofilm are easily targeted and destroyed by antibiotics. |
The main problem with biofilms is that antibiotics and many other treatments have a hard time penetrating the biofilm structure and killing the bacteria inside. This can make treatment very difficult and greatly increase the risk of recurring infections.
The National Institute for Health (NIH) says that biofilms are involved in up to 80% of all chronic, recurring infections. Yet, antibiotic drugs have little to no effect on biofilms.
In fact, antibiotics can actually drive disease-causing bacteria to form biofilms to protect themselves. Once you stop taking the antibiotics, the bacteria hiding in the biofilm can come back out again, causing another infection. If you have a history of recurring infections, then chances are high that a biofilm is involved.
Bacterial Resistance is Why Antibiotics Fail
Biofilms and the other bacterial resistance factors are well known to microbiologists. But unfortunately, these resistance factors are still a new area of research in the field of medicine. Antibiotic drugs are very simple chemically, so they are very easy for bacteria to figure out and defend against. And antibiotic development is focused solely on free floating bacteria, not on biofilms or L-forms. What's more, there are no commonly available tests to detect biofilms, L-forms and other ways that bacteria can hide in your body.
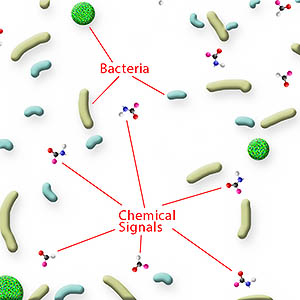 |
Bacteria share information with each other for mutual protection. If danger is lurking, signals are sent out to form a Biofilm, to produce spores, to increase virulence and other offensive and defensive measures. |
So the current mainstream treatments for infections are unable to address biofilms and other resistance factors. Even if an antibiotic does work, the bacteria can quickly learn how to resist it, or go into hiding until the antibiotic is stopped. These challenges are why recurring infections are such a problem with C. difficile and why antibiotics often fail to treat it.
In addition to biofilms, bacteria also use chemical signals called quorum sensing to communicate with each other and resist antibiotics. If one bacteria senses a danger, it can send warning signals to neighboring microbes. This allows different bacteria to coordinate to protect each other.
Another way bacteria resist antibiotics is through efflux pumps. Bacteria use these tiny pumps imbedded into their cell walls to expel antibiotics and other harmful chemical agents. This keeps the antibiotic from reaching lethal concentrations inside the bacteria, helping them to survive.
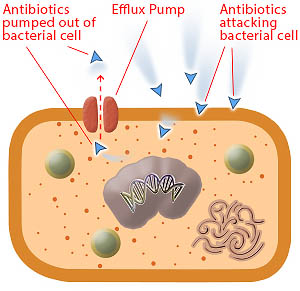 |
Bacteria use efflux pumps to expell antibiotic drugs from their cells before the drugs can kill the bacterial cell. |
Some kinds of bacteria can shed their cell walls entirely, becoming very tiny and hiding undetected inside your body for long periods of time. These L-forms, or cell wall deficient bacteria, are also called stealth bacterial. While L-forms have been isolated and researched and are suspected to cause recurring infections, few doctors have even heard of them.
Yet another way that some bacteria like C. difficile survive and resist treatments is by forming spores, which are protective shells. Unlike biofilms, which hold many bacteria, spores are formed separately around each individual bacterial cell. If biofilms are likened to a fortress protecting a whole army, then spores are like the armor that each individual soldier wears. But just like biofilms, spores protect bacteria from antibiotics and help them survive and hide in your body.
Nature Provides a Solution
Biofilms, spores, quorum sensing and other resistance factors are powerful ways that bacteria defend themselves against man-made antibiotic drugs. Thankfully, plants, herbs and trees have developed sophisticated chemical weapons and countermeasures to protect against attacks by bacterial, fungal and viral infections. And unlike antibiotic drugs, the defenses used by plants are complex mixtures of natural substances that work together on multiple levels, so bacteria can't easily develop resistance.
The good news is that you can use these plant-based weapons to help address your own infections. And there are specific plant-based remedies with confirmed activity against biofilms, efflux pumps and other bacterial resistance factors. So using the right medicinal herb can help address the biofilms and other factors that contribute to recurring infections and antibiotic drug failures.
The Power of Herbal Blends
Combining more than one medicinal herb together into a single formula can provide broad and powerful activity against infections. For example, herbs with biofilm busting properties can be blended with herbs that target quorum sensing. Ingredients that help remove dead biofilm debris and bacterial toxins can also be added. And herbs that reduce gut inflammation can be blended with herbs that promote tissue healing and regeneration.
 |
Blending multiple herbs together can provide unique benefits beyond any single herb by itself. |
A well known example is garlic. Garlic contains 27 known active ingredients and at least 35 other ingredients, but allicin is the best known and the most studied. Allicin can interrupt quorum sensing and a recent study showed garlic inhibits C. difficile growth from spores.
Another example is oregano oil. A key ingredient of oregano called carvacrol reduces the number of spores that C. difficile bacteria make. Oregano also acts against efflux pumps, L-forms stealth bacteria and biofilms.
Olive leaf extract has potent and broad-spectrum antimicrobial, antiviral and antifungal properties. Oleuropein, a key component, protects olive trees from insects and bacteria. Besides it's powerful antibacterial properties, olive leaf also has immune stimulating effects and anti-inflammatory properties. And it has a good safety record and lack of side effects.
The CD Herbal Detox Kit
 |
The CD Herbal Detox Kit combines three products for broad-acting support against all kinds of bacterial resistance. |
The three formulas inside the CD Herbal Detox Kit were specifically selected for the broadest possible support for C. difficile infections and its resistance factors. This kit combines olive leaf, garlic, oregano oil and other medicinal herbs into two separate herbal blends called Olivirex and Biocidin. The kit also includes GI Detox+, which contains a combination of ingredients to help your body remove C. difficile toxins A and B, along with other toxic bacterial byproducts.
Get the CD Herbal Detox Kit today, along with a detailed usage guide, by clicking here, or by clicking on the image to the right.
Photo credits: Biofilm: PHIL Janice Carr. Herbs: © Studio Barcelona/Fotolia.com


