If you’re taking antibiotics, there are some important things you need to know…

Last medically reviewed and updated: November 2025. Information based on current IDSA/SHEA and ACG guidelines for C. difficile infections.
When you’re facing a C. difficile infection, it’s natural to feel unsure about antibiotics — especially if antibiotics caused the problem in the first place. The truth is, only a few antibiotics still work well for C. diff, and treatment recommendations have changed in recent years. Understanding which ones doctors now prefer, what their side effects are, and how to rebuild your gut afterward can help you make better decisions and avoid another relapse.
Below you’ll find the most up-to-date information on C. diff antibiotics, what’s new for 2025, and how to recover your gut health once treatment is over. Everything here is drawn from official medical guidelines and my 20+ years of research and real-world experience helping people overcome gut infections naturally.
The Latest Antibiotic Treatments for C. diff
Due to antibiotic resistance and effectiveness, only a handful of antibiotics are used today for Clostridioides difficile.
The main options are fidaxomicin (Dificid) and vancomycin, both taken by mouth. Metronidazole (Flagyl) is no longer recommended as a first choice and is usually reserved for mild cases when other drugs aren’t available [1,2].
Top 3 Antibiotic Choices for C. difficile
- First episode (non-severe or severe): Fidaxomicin is now the preferred antibiotic because it lowers the risk of relapse; oral vancomycin is still a good alternative [1,2].
- Recurrence: Either fidaxomicin (standard or extended-pulsed) or a vancomycin taper/pulse regimen is used. Some doctors may also follow vancomycin with rifaximin (“rifaximin chaser”) [1].
- Fulminant (life-threatening) cases: High-dose oral or nasogastric (NG) vancomycin together with IV metronidazole. In some cases, rectal vancomycin is added if the gut is blocked [3].
2025 Treatment Updates:
- Bezlotoxumab (Zinplava)—an IV antibody once used to prevent relapse—was discontinued in the U.S. as of January 31, 2025 [7].
- Microbiome-based therapies are now FDA-approved to help prevent recurrence after antibiotics:
- VOWST — oral capsule microbiota spores [5]
- REBYOTA — single-dose enema microbiota product [6]
Antibiotic choices and dosing vary by age, severity, and local resistance patterns. These recommendations follow current U.S. guidelines and 2025 clinical data. Always review options with your healthcare provider.
Antibiotics and FMT: Pros, Cons, and Real-World Results
Here’s what studies — and real-world experience — show about how well these treatments work.
Antibiotics

While antibiotics are the standard medical treatment for C. diff, they aren’t always a long-term fix. Even with the best options like fidaxomicin and vancomycin, research shows that about 20–25 % of people relapse after the first infection, and the relapse rate can climb higher after each recurrence. [1,8,9]
- Pros: They can stop the overgrowth quickly, relieve symptoms, and are sometimes life-saving in severe or life-threatening cases.
- Cons: They also wipe out helpful gut bacteria, which is one reason relapses are so common. Each round may further disrupt the microbiome and increase antibiotic resistance.
Also see: Top 5 Antibiotics That Cause C. diff →
FMT and Microbiome Therapies
FMT and microbiome-based therapies can be highly effective for people who don’t respond to antibiotics. Studies show that these treatments successfully stop recurrent C. diff infections in 70–90% of patients, but about 10–30% may still relapse over time, depending on health status and treatment method. [5,6] While results are encouraging, FMT and microbiome therapies aren’t a guaranteed cure, and not every patient is an ideal candidate.
- Pros: FMT and FDA-approved microbiome products like VOWST and REBYOTA can restore beneficial bacteria and lower relapse risk after antibiotics.
- Cons: They’re not perfect either. Success rates vary, and while generally safe, FMT carries a small risk of infection transfer or immune reaction. I cover this more here: Fecal Transplants Pros and Cons →.
That’s why rebuilding your gut’s balance after any antibiotic or FMT is so important. Nourishing your microbiome through smart food choices, hydration, and targeted probiotic and toxin binder support can help you stay on the path to lasting recovery.
Watch: Combining Medical and Microbiome Therapies
VOWST, FMT & Probiotics – Is It Safe to Combine Them?
In this short video, I explain how medical and natural treatments can work together — and what to know about adding probiotics after antibiotics, FMT, or microbiome therapies like VOWST.
Getting Through Antibiotics and Bouncing Back
If you’ve taken antibiotics for C. diff, there are two key steps:
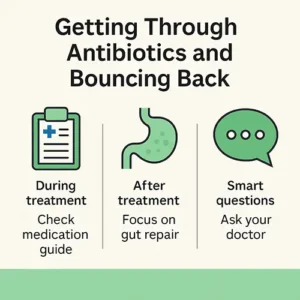
- During treatment: Check your medication guide for food or drug interactions. Ask your doctor what’s next if symptoms don’t improve.
- After treatment: Focus on gut repair—reintroducing beneficial microbes, restoring digestion, and reducing relapse risk. In repeat cases, ask whether a microbiome product such as VOWST or REBYOTA is appropriate [5,6].
Smart questions to ask your doctor:
- “Is fidaxomicin an option for me? If not, why vancomycin?” [1,2]
- “If it returns, what’s your plan—fidaxomicin again, or a vancomycin taper?” [1]
- “If it’s severe, what emergency antibiotics will be used?” [3]
- “Could a microbiome therapy help keep it from coming back?” [5,6]
Reducing Relapse Risk
From my experience as a microbiologist and educator helping thousands of people recover from resistant infections and C. diff since 2007, I’ve seen that rebuilding the gut microbiome after antibiotic therapy is often the turning point for long-term gut recovery. Supporting digestion with targeted probiotics, nutrient balance, and immune health during this phase can greatly reduce relapse risk.
Other Standard Medical Treatments for C. difficile Infections
Fecal microbiota transplantation (FMT) is still used when antibiotics fail, but standardized FDA-approved microbiome therapies (above) are now preferred in many cases [5,6]. If you’re considering FMT, be aware of its potential risks and recent safety alerts — infection risks are covered here: Fecal Transplant Causes Deadly Infection →.
FMT and microbiome therapies are evolving fast, so checking that your provider uses screened, FDA-compliant donor material is key.
As research evolves, many doctors are combining traditional antibiotic therapy with microbiome restoration and probiotics — an approach I’ve found to be very effective in my clinical collaborations and community work since 2007.
Frequently Asked Questions
What’s the best antibiotic for C. diff in 2025?
Fidaxomicin is now the preferred first-line antibiotic for most adults, with vancomycin as an accepted alternative.
Can probiotics help prevent C. diff relapse?
Many people use spore-based probiotics or microbiome restoration therapies after antibiotics to reduce recurrence risk.
Is fecal microbiota transplantation (FMT) still used for C. diff?
FMT is still an option when antibiotics fail, but FDA-approved microbiome products like VOWST and REBYOTA are now preferred for preventing recurrences.
Get the Full Picture on C. diff Recovery
C. diff is serious, but you do have options. Learn about natural and probiotic approaches that support gut microbiome recovery:

About the Author – Michelle Moore, BSc
Michelle Moore is a microbiologist, holistic health educator, and author of C. difficile Treatments & Remedies. With pharmaceutical research experience and over 20 years in natural medicine, she helps people recover from C. diff and other chronic infections naturally.
Reviewed and updated: November 2025 to reflect the most recent C. difficile treatment guidelines and microbiome research.
References
- IDSA/SHEA 2021 Focused Update on C. difficile Treatment (Guidelines for Adults and Children).
- ACG Clinical Guideline 2021 – Management of C. difficile Infection in Adults.
- Management of Fulminant C. difficile Infection (Oral/NG Vancomycin + IV Metronidazole).
- Comparative studies showing fidaxomicin’s lower recurrence rates vs vancomycin.
- FDA approval of VOWST (oral microbiota spores) for recurrence prevention after antibiotics.
- FDA approval of REBYOTA (enema microbiota product) for recurrence prevention after antibiotics.
- Bezlotoxumab (Zinplava) discontinuation notice – U.S. market withdrawn January 31, 2025.
- Kelly CP. Can we identify patients at high risk of recurrent Clostridium difficile infection? Clin Microbiol Infect. 2012;18(Suppl 6):21–27.
- Lessa FC, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825–834.
This page is for educational purposes only and is not a substitute for medical advice. Always work with your healthcare provider to determine the best treatment for your situation.


 Fill in the form below to get our C. diff. tips newsletter and your free report “10 Things You Need to Know to Overcome C. difficile”.
We value your Privacy. Your email will be kept strictly confidential & secured. See our
Fill in the form below to get our C. diff. tips newsletter and your free report “10 Things You Need to Know to Overcome C. difficile”.
We value your Privacy. Your email will be kept strictly confidential & secured. See our